KEY POINTS
- Research into the menstrual cycle and exercise/sport has been ongoing for more than a century yet, to date, no consensus has been reached in this regard.
- The relationship between menstrual cycles and exercise/sport is multifactorial and bi-directional.
- Menstrual cycles are highly variable and personal and as such should be approached on an individual, rather than a population, basis.
- The quality of past research should be assessed before translation into practice and future research should adopt a high-quality approach.
- Unsubstantiated interventions, such as menstrual cycle phase-based training programmes, should not be adopted at this time despite their popularity in practice and social media settings.
NOTE FROM THE AUTHOR
The article is written about cisgender women [i.e., someone who was assigned female at birth and identifies as a woman]. I have used the word female as an adjective [i.e., characteristic of girls, women, or the female sex: exhibiting femaleness] and the word woman as a noun [i.e., denoting an adult female human]. The terms sportswomen and female athletes are used interchangeably. When describing the work of others, I have adopted the language used by the authors themselves to describe their own work.
INTRODUCTION
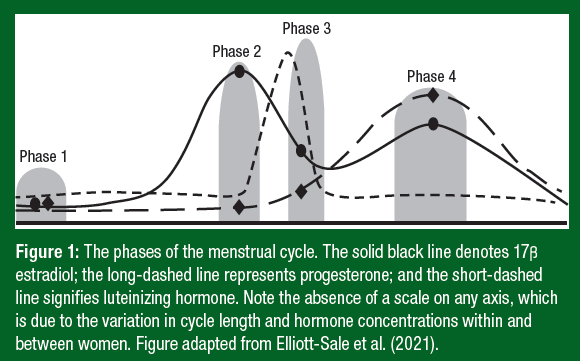
Sexual reproduction is one of the most notable sex differences. During puberty girls experience menarche (i.e., first menstrual period in a female adolescent - typically occurring around 12 years of age), which signals the ‘official start’ of the menstrual cycle and persists until menopause (i.e., cessation of menstrual periods - typically occurring around 50 years of age). The menstrual cycle is an infradian (i.e., lasting longer than one day), circamensal (i.e., lasting approximately one month) biological rhythm. Biological rhythms are recurring, endogenous cycles that are usually attuned to internal and external cues. During the menstrual cycle, the ovarian hormones estrogen and progesterone fluctuate in a predictable repeating pattern as shown in Figure 1, although it should be noted that there is large inter- and intra-individual variability in cycle length and hormone levels.
Aside from their paradigmatic roles, estrogen and progesterone have been shown to have non-reproductive functions; for example, they can affect the skeleton, heart and brain. As such, the menstrual cycle [more specifically the hormones estrogen and progesterone] has developed into a topic of interest for female athletes from a health and performance perspective.
RESEARCH TIMELINE
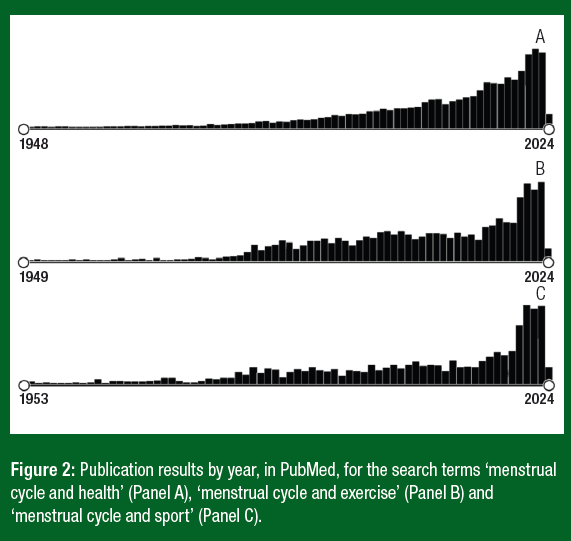
Mainstream research investigating the menstrual cycle and health (Figure 2. Panel A), exercise (Figure 2. Panel B) and sport (Figure 2. Panel C) first emerged in the late 1940’s / early 1950’s. Starting topics included ‘Tampon protection and menstrual health in industry’ [representing health-based research], ‘Billig exercises for dysmenorrhea’ [representing exercise-based research], and ‘Reduction of muscular performance during menstruation’ [representing sport-based research]. Whilst menstrual cycle health-based research has grown steadily over time, there has been two distinct increases in menstrual cycle and exercise/sport-related research; first in the early 1980’s and then again in the 2020’s, with annual outputs almost doubling between 2019 and 2020. Historically, research related to menstrual cycles and female athletes can be classified into five principal areas:
- The effects of menstruation (i.e., the physical act of bleeding) on athletic performance.
- The effects of exercise/sport on menstrual [dys]function (e.g., menstruation and ovulation).
- The effects of exercise/sport on menstrual cycle symptoms (e.g., dysmenorrhea).
- The effects of menstruation (i.e., the physical act of bleeding) on athletic performance.
- The effects of exercise/sport on menstrual [dys]function (e.g., menstruation and ovulation).
- The effects of exercise/sport on menstrual cycle symptoms (e.g., dysmenorrhea).
This Sports Science Exchange (SSE) article will chart the evolution of research in these key areas over the last century.
MENSTRUATION AND ATHLETIC PERFORMANCE
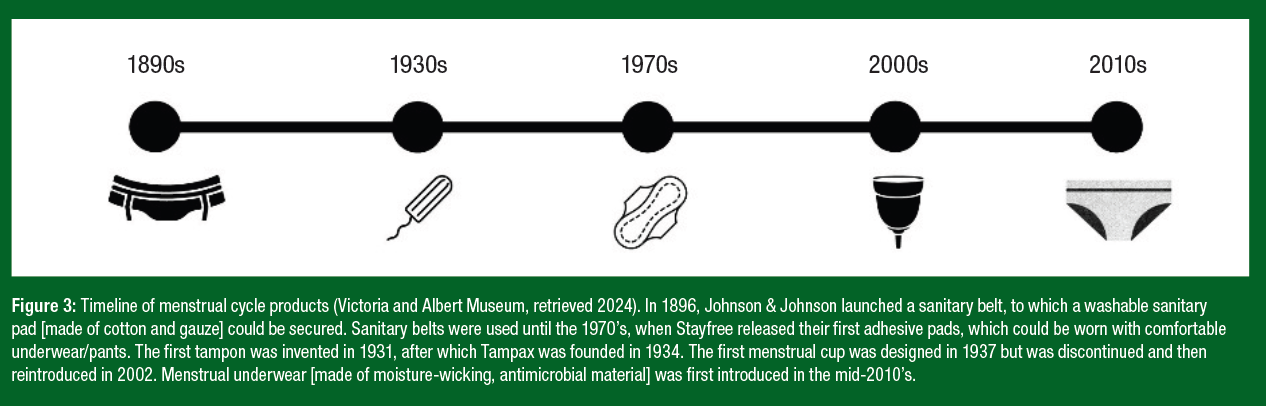
The design, accessibility and affordability of menstrual products will likely influence a female athletes experience of menstruation whilst training or competing. Figure 3 shows the evolution of sanitary products, highlighting the products that female athletes have been using over the last century (i.e., adhesive sanitary pads, tampons, menstrual cups and period pants). Some female athletes have reported feel distracted, anxious and lacking confidence during menstruation, due to fear of leaking or flooding onto their clothing (Adam et al., 2022). As such, it is likely that menstruation (i.e., Phase 1 of the menstrual cycle, when concentrations of estrogen and progesterone are at their lowest), is capable of affecting some female athletes and their athletic performance, although the reach (i.e., how many female athletes) and impact (i.e., how much they are affected) of this phenomenon is currently unknown. This topic warrants further investigation and possible changes to practice and policies; for example, free, readily available and fit-for-purpose sanitary products for female athletes and an increased awareness and knowledge about menstruation in a sporting context.
EXERCISE/SPORT AND MENSTRUAL [DYS]FUNCTION
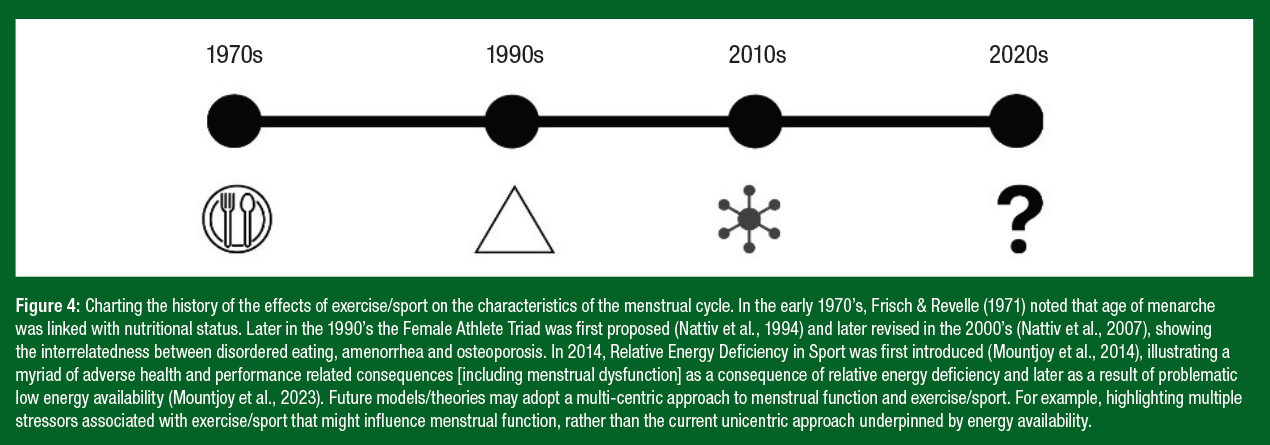
Certain types of menstrual dysfunction have been linked with exercise/ sport; for example, anovulation, luteal phase deficiency, oligomenorrhea and amenorrhea. Exercise/sport may result in menstrual dysfunction due to a variety of reasons linked with metabolic and/or psychogenic stress (Pauli & Berga, 2010). Figure 4 shows the timeline of research investigating the possible effects of exercise/sport on menstrual function, which has been mainly grounded in metabolic stress (i.e., dietary energy intake and exercise energy expenditure).
EXERCISE/SPORT AND MENSTRUAL SYMPTOMS
Symptoms are defined as ‘something that a person feels or experiences’. As such, there are many methodological issues and challenges associated with symptoms reporting, for example subjectivity, recall and individuality, make research in this area difficult to group and interpret. Dysmenorrhea (i.e., painful periods) is one of the most commonly reported menstrual cycle symptoms/disorders, with 32% (range 8-86%) of a recently sampled athletic population stating that they have experienced this condition (Taim et al., 2023). From the 1940’s to the present day, many athletes have reported relief from dysmenorrhea during a range of activities from stretching to intensive exercise (Billig, 1943; Golub, 1959; Dehnavi et al., 2018). Indeed, a systematic review and Bayesian network meta-analysis published in 2024 concluded that exercise could be considered as a potentially effective non-pharmacological treatment (Li et al., 2024). Notwithstanding these findings, other research has not shown any beneficial effects of exercise on dysmenorrhea (Locke & Warren, 1999) and consequently the efficacy of such interventions warrants further investigation with better procedural standards to overcome previous methodological flaws.
Similarly, there has been some evidence (Aganoff & Boyle, 1994; Randeva et al., 2002; Vishnupriya et al., 2012) over the last 30 years, to suggest that exercise can alleviate the symptoms of pre-menstrual syndrome (i.e., the name for the symptoms women can experience in the weeks before their period). However, this topic still requires further high-quality studies (i.e., randomized controlled trials) to confirm this response and to determine the most efficacious exercise interventions. At present, there is a paucity of evidence to support that claim that exercise reduces the frequency and/or severity of pre-menstrual syndrome and/or primary dysmenorrhoea (Daley, 2009).
MENSTRUAL CYCLE AND EXERCISE PERFORMANCE
Since the 1970’s (Hansen & Weeke, 1974; Petrofsky et al., 1976) the question of whether the menstrual cycle affects exercise/sport performance has been the subject of much debate, with the biggest surge in interest seen in the last 2-3 years (i.e., 2020-2023). For example, some [menstrual] cycle syncing workouts (i.e., where you train according to which phase of the menstrual cycle you are in) on Tik Tok have been viewed more than 2.2 million times. This research question relates to the non-reproductive actions of cyclical estrogen and progesterone and their ability to affect other physiological systems in a significant/meaningful way, resulting in a net change in athletic performance. This means that, following their reproductive functions, any remaining estrogen and progesterone exert a biological action on other tissues around the body to such an extent as to acutely (i.e., in the case of the menstrual cycle) affect exercise/sport performance. For a complete overview (i.e., systematic review and meta-analysis) of research in this area see McNulty et al. (2020). At present, there is insufficient high-quality evidence (51 eligible primary outcome studies, 8% high quality; McNulty et al., 2020) to answer this research question, although it should be noted that an absence of evidence, is not evidence of absence.
Over the last decade, numerous programmes (e.g., apps, books, digital content) have been developed that advise female exercisers/ athletes on the effects of the menstrual cycle on training responses and adaptations, nutrition, injury risk, symptomology, athletic performance, etc.. In general, these programmes assume universal responses despite the known heterogeneity associated with all aspects of the menstrual cycle and are based on insufficient, low-quality datasets (Colenso- Semple et al., 2023). Until a consensus, on the effects of cyclical changes in estrogen and progesterone across the menstrual cycle has been reached, generalized programming based on menstrual cycle phases is premature, misleading and irrelevant. Moreover, it must be noted that these programmes are often based on assumed rather than verified menstrual cycle phases, meaning that, in addition to prescribing non-evidence informed practices, these programmes are based on uncorroborated phases - based on bleeding patterns alone - thereby conflating several dysfunctional profiles with eumenorrheic cycles. For a visual representation of eumenorrheic to amenorrheic hormonal profiles see Allaway et al. (2016). Tailoring exercise/sport in line with personal lived experiences of the menstrual cycle is however advisable, as this approach is responsive to the individual rather than based on a currently hypothetical, unsubstantiated, communal response.
MENSTRUAL CYCLE SYMPTOMS AND EXERCISE PERFORMANCE
Leaving aside the potential biological effects of estrogen and progesterone on other non-reproductive tissues, these hormones have been associated with symptoms (i.e., something that a person feels or experiences), which are grouped as physical and emotional responses and are collectively known as changes in well-being (i.e., ‘feeling good and functioning well’). Over the last decade, numerous authors have audited the self-reported prevalence of menstrual cycle symptoms and their perceived impact on exercise/sport performance in a variety of sports (Heyward et al., 2022; Martin et al., 2018; Nolan et al., 2023; Parker et al. 2022; Taim et al., 2024). For example, Martin et al. (2018) reported that 77% of non-hormonal contraceptive using athletes reported negative side effects associated with their menstrual cycle, primarily during days 1-2 of menstruation (82%). In addition, Taim et al. (2024) stated that 62% and 67% of non-oral contraceptive pill using athletes perceived that their menstrual cycles affected their ability to train and compete. It is, however, difficult to interpret this research due to numerous methodological issues, such as: inconsistent research design and protocols; bias (e.g., recall and reporting); lack of validated tools/measures; the absence of longitudinal datasets; and unverified outcomes. At present, most changes in well-being, in non-hormonal contraceptive using female athletes, are being attributed to the menstrual cycle, however, in order to be considered as ‘menstrual cycle symptoms’ any reported effects need to be observed across multiple, consecutive menstrual cycles in order for their cyclicity to be recognized. Indeed, other probable causes for these changes in well-being need to be ruled out before any symptoms can be linked with menstrual cycle phase (i.e., often these symptoms will be a diagnosis of exclusion).
HISTORICAL, CURRENT OR FUTURE HOT TOPIC?
Despite its current popularity, the issue of the menstrual cycle and ‘performance’ has been contemplated beyond the last century. In 1876, Dr. Mary Jacobi won the Boylston Prize at Harvard University for her essay on menstrual cycles and occupational performance, in which she (i) refuted the supposed physical limitations of women described by Dr. Edward H. Clarke's publication Sex in Education; or A Fair Chance for the Girls (1873) and (ii) concluded that “nothing in the nature of menstruation to imply the necessity, or even the desirability, of rest for women whose nutrition is really normal.” As such, Dr Jacobi dispelled - more than one hundred years ago - the myth that menstrual cycles dictate [occupational] performance when women are adequately fuelled (i.e., in the absence of low energy availability). Fifty years after Dr Jacobi’s essay, renowned gynaecologist Ludwig Frankel commented that “the only regularity of the menstrual cycle is its irregularity” (Vitzthum, 2021), making him amongst the first to comment on the methodological challenges faced by researchers both then and today. Presently, Elliott-Sale et al. (2021) have proposed a number of methodological considerations to aid (i.e., improve the methodological quality) with research investigating the effects of the menstrual cycle, amongst other ovarian hormone profiles, on a variety of sport and exercise outcomes. Using these considerations, Elliott-Sale et al . (2023a, b) have formed an international, multisite, innovation project to investigate the effects of menstrual cycle phase on aspects of exercise physiology in female athletes, with the aim of delivering a high-quality, adequately powered, independently replicated dataset. In the future, consideration should be given to more (i.e., other than menstrual cycle) ovarian hormone profiles, such as hormonal contraceptives, pregnancy and menopause, as many female athletes also experience these hormonal states (Martin et al., 2018).
PRACTICAL APPLICATIONS
The goal of menstrual cycle research is to facilitate optimal health and athletic performance on any day of the menstrual cycle. As such the following practical applications are proposed:
- Offer accessible (ideally free) fit-for-purpose sanitary products to female exercisers and athletes in their training and competitive environments.
- Keep track of menstruation and menstrual cycle length, in order to allow female exercisers and athletes to know when to expect their periods and to plan accordingly.
- Establish, rather than assume, menstrual cycle phases, in order to allow female exercisers and athletes to overlay any changes in well-being (i.e., symptoms), injury, performance, etc. against their individual phases, in order to investigate if (i.e., not all women will be affected) and/or how (i.e., positively or negatively) they are affected and to plan/adapt accordingly if necessary.
- Be critical of research publications and social media, to ensure that female exercisers and athletes have access to a body of credible, trustworthy, high-quality evidence to inform their practice.
- Fuel for the demands of the activity/sport, in order to maintain all physiological processes including reproduction.
SUMMARY
Despite more than a century of research, little is known about the relationship between the menstrual cycle and exercise/sport. This relationship is likely to be multi-factorial and bidirectional. It is plausible that, given the variability associated with all aspects of the menstrual cycle (e.g., characteristics and responses), a universal blueprint is not feasible or warranted, instead an individual approach to the menstrual cycle should be adopted. This will ensure that those affected by their menstrual cycle will be identified and offered an appropriate bespoke intervention, thus ensuring that - often limited - resources are not diluted by unnecessary and unsubstantiated global dictates.
The views expressed are those of the authors and do not necessarily reflect the position or policy of PepsiCo, Inc.
REFERENCES
Adam, M.E.K., A. Bristow, K.C. Neely, and M.C. Erlandson (2022). Do women athletes’ experiences of menstrual function and dysfunction vary across competition levels? A mixed methods exploration. Psych. Sport Exerc. 63:102270.
Aganoff, J.A., and G.J. Boyle (1994). Aerobic exercise, mood states and menstrual cycle symptoms. J Psychosom Res. 38:183-192.
Allaway, H.C., E.A. Southmayd, and M.J. De Souza (2016). The physiology of functional hypothalamic amenorrhea associated with energy deficiency in exercising women and in women with anorexia nervosa. Horm. Mol. Biol. Clin. Invest. 25:91-119.
Billig, H.E. (1943). Dysmenorrhea: the effects of a postural defect. Arch. Surg. 46:611–613.
Clarke, E.H. (1873) Sex in education; or fair chance for the girls. JR. Osgood and Company.
Colenso-Semple, L.M., A.C. D'Souza, AC, K.J. Elliott-Sale, and S.M. Phillips (2023). Current evidence shows no influence of women's menstrual cycle phase on acute strength performance or adaptations to resistance exercise training. Front. Sports Act. Living 5:1054542.
Daley, A. (2009). The role of exercise in the treatment of menstrual disorders: the evidence. Br. J. Gen. Pract. 59:241-242.
Dehnavi, Z.M., F. Jafarnejad, and Z. Kamali (2018). The effect of aerobic exercise on primary dysmenorrhea: A clinical trial study. J. Educ. Health Promot. 7:3.
Elliott-Sale, K.J., C.L. Minahan, XAKJ de Jonge, K.E. Ackerman, S. Sipilä, N.W. Constantini, C.M. Lebrun, and A.C. Hackney (2021). Methodological considerations for studies in sport and exercise science with women as participants: A working guide for standards of practice for research on women. Sports Med. 51:843-861.
Elliott-Sale, K.J., K.E. Ackerman, C.M. Lebrun, C. Minahan, C. Sale, T. Stellingwerff, P.A. Swinton, and A.C. Hackney (2023a). Feminae: an international multisite innovative project for female athletes. BMJ Open Sport Exerc. Med. 9:e001675.
Elliott Sale, K.J., T.R. Flood, S.M. Arent, E. Dolan, B. Saunders, M. Hansen, J.K. Ihalainen, R.S. Mikkonen, C. Minahan, J.S. Thornton, K.E. Ackerman, C.M. Lebrun, C. Sale, T. Stellingwerff, P.A. Swinton, and A.C. Hackney (2023b). Effect of menstrual cycle and contraceptive pill phase on aspects of exercise physiology and athletic performance in female athletes: protocol for the Feminae international multisite innovative project. BMJ Open Sport Exerc. Med. 9:e001814.
Frisch, R.E., and R. Revelle (1971). Height and weight at menarche and a hypothesis of menarche. Arch. Dis. Childhood 46:695-701.
Golub, L.J., (1959). A new exercise for dysmenorrhoea. Am. J. Obst. Gynecol. 78:152-155.
Hansen, A.P., and J. Weeke (1974). Fasting serum growth hormone levels and growth hormone responses to exercise during normal menstrual cycles and cycles of oral contraceptives. Scand. J. Clin. Lab. Invest. 34:199-205.
Heyward, O., K.J. Elliott-Sale, G. Roe, S. Emmonds, K. Hornby, K.A. Stokes, and B. Jones (2022). Oral contraceptive use in Premiership and Championship women's rugby union: perceived symptomology, management strategies, and performance and wellness effects. Sci. Med. Footb. 22:1-8.
Jacobi, M.P. (1877). The question of rest for women during menstruation. New York: G.P. Putnam's Sons.
Li, X., X. Hao, J.H. Liu, and J.P. Huang (2024). Efficacy of non-pharmacological interventions for primary dysmenorrhoea: a systematic review and Bayesian network meta-analysis. BMJ Evid Based Med. doi: 10.1136/bmjebm-2023-112434. Online ahead of print.
Locke, R.J., and M.P. Warren (1999). Curbside consult: What is the effect of exercise on primary dysmenorrhea? West. J. Med. 171):264-265.
Martin, D., C. Sale, S.B. Cooper, and K.J. Elliott-Sale (2018). Period prevalence and perceived side effects of hormonal contraceptive use and the menstrual cycle in elite athletes. Int. J. Sports Physiol. Perform. 13:926-932.
McNulty. K.L., K.J. Elliott-Sale, E. Dolan, P.A. Swinton, P. Ansdell, S. Goodall, K. Thomas, and K.M. Hicks (2020). The effects of menstrual cycle phase on exercise performance in eumenorrheic women: A systematic review and meta-analysis. Sports Med. 50:1813- 1827.
Mountjoy, M., J. Sundgot-Borgen, L. Burke, S. Carter, N. Constantini, C. Lebrun, N. Meyer, R. Sherman, K. Steffen, R. Budgett, and A. Ljungqvist (2014). The IOC consensus statement: beyond the Female Athlete Triad--Relative Energy Deficiency in Sport (RED-S). Br. J. Sports Med. 48:491-497.
Mountjoy. M., K.E. Ackerman, D.M. Bailey, L.M. Burke, N. Constantini, A.C. Hackney, I.A. Heikura, A. Melin, A.M. Pensgaard, T. Stellingwerff, J.K. Sundgot-Borgen, M.K. Torstveit, A.U. Jacobsen, E. Verhagen, R. Budgett, L. Engebretsen, and U. Erdener (2023). International Olympic Committee's (IOC) consensus statement on Relative Energy Deficiency in Sport (REDs). Br. J. Sports Med. 57:1073-1097.
Nattiv, A., R. Agostini, B. Drinkwater, and K.K. Yeager (1994). The female athlete triad. The inter-relatedness of disordered eating, amenorrhea, and osteoporosis. Clin. Sports Med. 13:405-418.
Nattiv, A., A.B. Loucks, M.M. Manore, C.F. Sanborn, J. Sundgot-Borgen, and M.P. Warren (2007). American College of Sports Medicine position stand. The female athlete triad. Med. Sci. Sports Exerc. 39:1867-1882.
Nolan, D., K.J. Elliott-Sale, and B. Egan (2023). Prevalence of hormonal contraceptive use and reported side effects of the menstrual cycle and hormonal contraceptive use in powerlifting and rugby. Phys. Sportsmed. 51:217-222.
Parker. L.J., K.J. Elliott-Sale, M.P. Hannon, J.P. Morton, and G.L. Close (2022). An audit of hormonal contraceptive use in Women's Super League soccer players; implications on symptomology. Sci. Med. Footb. 6:153-158.
Pauli, S.A., and S.L. Berga (2010). Athletic amenorrhea: energy deficit or psychogenic challenge? Ann. NY Acad. Sci. 1205:33-38.
Petrofsky, J.S., D.M. LeDonne, J.S. Rinehart, and A.R. Lind (1976). Isometric strength and endurance during the menstrual cycle. Eur. J. Appl. Physiol. 35:1-10.
Randeva, H.S., K.C. Lewandowski, J. Drzewoski, K. Brooke-Wavell, C. O'Callaghan, L. Czupryniak, E.W. Hillhouse, and G.M. Prelevic (2002) Exercise decreases plasma total homocysteine in overweight young women with poly cystic ovary syndrome. J. Clin. Endocrinol. Metab. 87:4496–4501.
Taim, B.C., C. Ó Catháin, M. Renard, K.J. Elliott-Sale, S. Madigan, and N. Ní Chéilleachair (2023). The prevalence of menstrual cycle disorders and menstrual cycle-related symptoms in female athletes: A systematic literature review. Sports Med. 53:1963- 1984.
Taim, B.C., J. Lye, H.T. Suppiah, T.W. Chan, M. Chia, and A. Clarke (2024). Menstrual cycle characteristics, perceived impact on performance, and barriers to communication: Perspectives of high-performance adolescent athletes in Singapore. Scand. J. Med. Sci. Sports 34:e14488.
Victoria and Albert Museum. https://www.vam.ac.uk/ articles/a-brief-history-of-menstrual-products#:~:text=The%20use%20of%20 menstrual%20care,to%20make%20homemade%20cloth%20pads (retrieved 15.02.24)
Vishnupriya, R., and P. Rajarajeswaram (2011). Effects of aerobic exercise at different intensities in premenstrual syndrome. J. Obstet. Gynaecol. India 61:675-682.
Vitzthum, V. (2021), Field methods and strategies for assessing female reproductive functioning. Am. J. Hum. Biol. 33:e23513.