Key Points
- Energy intake needs to match energy expenditure to maintain a high level of training, building and repair of body tissues, cover the energy costs of daily living, prevent illness and maintain reproductive function.
- Low energy intakes increase the risk of fatigue, injuries and illness, poor nutritional status, menstrual dysfunction, lack of improvement in performance and/or difficulty training at high intensities, and impairments in metabolic rate, immunity, protein synthesis and cardiovascular health.
- For active females, energy intakes less than 1,800 kcal/d make it difficult to get the dietary nutrients required for energy metabolism, maintenance of bone and blood, and general health.
- Eating enough carbohydrate to match the energy demands of sport will assure adequate glycogen replacement and the potential for high-level performance.
- Adequate protein is necessary for maintaining and repairing muscle and bone, and good health. Protein needs can range from 1.2-2.0 g/kg body weight per day and intake should be spread throughout the day.
- Female athletes who energy restrict or follow specialty diets are most likely to have low protein intakes. To preserve lean tissue during periods of energy restriction, protein intake (g/kg body weight) needs are greater than during periods of energy balance.
- The micronutrients most likely to be low in the diets of active women are iron, zinc, calcium, vitamin D and the B-vitamins (folate, B-6, thiamin, riboflavin) especially if energy is restricted, poor food choices are made, or gastrointestinal issues are present.
INTRODUCTION
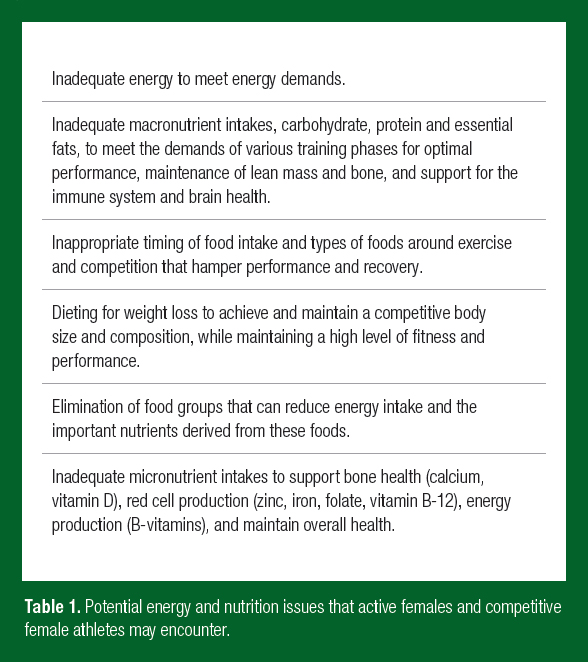
Active females and competitive female athletes have unique energy and nutrition issues compared to their male counterparts. The most common nutrition issues center around getting adequate energy to meet the energy demands of sport, activities of daily living, and reproduction, and selecting appropriate foods to get the nutrients required to support high levels of physical activity, building and repair of bone and muscle, and overall health (Table 1). Adolescent female athletes can face even larger energy and nutrition challenges due the need for energy and nutrients for growth and maturation, while having limited knowledge about appropriate food selection for sport and weight management, and a dependency on others to help provide food. Regardless of the age of the athlete, adequate food and nutrients must be consumed in the approp-riate amounts and at the appropriate times for health and performance to be optimal. Thus, health professionals who work with active females need to monitor energy and nutrition intakes to help prevent any health-related issues due to low or inappropriate intakes. The key energy and nutrient issues most like to occur in the female athlete are reviewed in this Sports Science Exchange article.
ENERGY NEEDS
Research frequently reports that female athletes have energy intakes that do not match their high level of energy expenditure. Based on doubly labeled water assessments of total energy expenditure, the energy needs of female athletes can vary widely depending on their sport (2,500-5,000 kcal/d) (Hill & Davies, 2001, 2002; Schulz et al., 1992; Sjodin et al., 1994). However, despite high-energy needs, many female athletes restrict energy intake to lose body fat to improve performance or to achieve a desired body size (Manore, 2015; Sundgot- Borgen & Garthe, 2011). Without adequate energy intake, wise food selection, and appropriate timing of food and fluid intake, nutrient intakes may be inadequate to maintain health and performance. When energy intakes drop below 1,800 kcal/d, it is difficult to obtain adequate nutrients (protein, carbohydrate, essential fatty acids and micronutrients) to maintain health, especially when expending high amounts of energy in exercise (Manore, 2002). Active females exercising 6-10 h/week typically need ~2,500 kcal/d or more to maintain body weight (Cialdella- Kam et al., 2014; Gilliat-Wimberly et al., 2001; Hand et al., 2016), while competitive female athletes who exercise 10-20 h/week or more can have energy needs > 3,000 kcal/d (Martin et al., 2002; Melin et al., 2015). If athletes report consuming less than these amounts, they may be underreporting energy intake (Schulz et al., 1992), restricting energy intake for weight/fat loss (Beals & Manore, 1998; Sundgot-Borgen et al., 2013), or are at risk for disordered eating or an eating disorder (Beals & Manore, 2002; Bratland-Sanda & Sundgot-Borgen, 2013; Sundgot-Borgen et al., 2013), or limiting certain foods for health or performance reasons (Cialdella-Kam et al., 2016).
If athletes have inadequate energy intake to match exercise energy expenditure, they are described as having “low energy availability” (EA) (Nattiv et al., 2007) or “relative energy deficiency in sport” (RED-S) (Mountjoy et al., 2014). RED-S describes a condition where an energy deficit occurs relative to the balance between energy intake (kcal/d) and total energy expenditure (kcal/d). The underlying cause of RED-S is low EA, and calculated by subtracting exercise energy expenditure (EEE, kcal/d) from total energy intake (kcal/d). Optimal EA is considered to be > 45 kcal/kg fat-free mass (FFM)/d, while low EA is considered to be < 30 kcal/kg/FFM/d (Nattiv et al., 2007). If overall energy intake is low, then EA may also be low. However, an athlete can have an energy intake that appears to match energy expenditure, while still having a low EA. In this situation, resting metabolic rate (RMR) may be suppressed due to energy restriction and be lower than predicted for sex, body size and activity level. EA can also change over a competitive season, so timing of measurements is critical. Although determining EA appears simple, it is much more difficult to get accurate measures of the other variables used in the calculation (Guebels et al., 2014). Energy intake needs to be measured as accurately as possible (observation, weighted food records, food pictures) over 7-10 days during training. If an individual is underreporting energy intake, then the assessment of EA will also be inaccurate (Guebels et al., 2014). Second, RMR and EEE should be measured and not estimated, since estimating these values introduces additional errors into the EA calculation. Finally, the activities that comprise EEE need to be defined (Guebels et al., 2014). Does EEE comprise only the energy expended during designated periods of sport training/competition, or does it include other physical activities outside of training? The health consequences of low energy intake or EA are discussed in the following section.
RELATIVE ENERGY DEFICIT
If the RED-S syndrome is present in an athlete, either inadvertently or through purposeful dieting or disordered eating, athletes can experience increased fatigue, injuries or illness, nutrient deficiencies, menstrual dysfunction, poor bone health, and lack of improvement in performance. In addition, athletes can experience impairments in metabolic rate, immunity, protein synthesis and cardiovascular health (Mountjoy et al., 2014). How do you know if an active female is consuming enough energy to meet energy demands? Below are highlighted some of the signs and symptoms of low energy intakes in active women. In addition, the International Olympic Committee Expert Panel has developed a RED-S clinical assessment tool (CAT) that can be used to help determine if an athlete is suffering from RED-S (Mountjoy et al., 2015).
- Exercise Associated Menstrual Dysfunction. When energy intake does not cover the demands of energy expenditure it may be manifested as oligomenorrhea (irregular periods) or amenorrhea (no period ≥ 3 months), especially during the training and competitive season (Nattiv et al., 2007). The irregularity or cessation of menses is a sign that the body does not have enough fuel for exercise and training, activities of daily living, and reproductive functions. If a female athlete is on oral contraceptives, it is important to know if she is using these because of menstrual irregularities. Remember, a female athlete does not have to have an eating disorder or disordered eating to have menstrual irregularities (Cialdella-Kam et al., 2014; Kopp-Woodroffe et al., 1999; Manore et al., 2007). Outside of other medical reasons, low EA, or energy intakes that do not match energy expenditures, appear to be the primary contributor to exercise associated menstrual dysfunction (Guebels et al., 2014; Nattiv et al., 2007). Determining why EA or energy intakes are low and how energy intakes may be improved is important, while still helping the athlete to maintain a reasonable weight and body composition. Current research shows that weight gain or an increase in body mass index (BMI, kg/m2) may be a predictor of renewed reproductive function (Arends et al., 2012; Cialdella-Kam et al., 2014). However, the restoration of reproduction function can and does take time. Retrospective and intervention research indicates that it may take one year or longer for normal reproductive function to return once energy balance issues are corrected (Arends et al., 2012; Cialdella- Kam et al., 2014). If low EA and menstrual dysfunction remain unchecked, they can lead to poor bone health (e.g., the Female Athlete Triad) (Nattiv et al., 2007).
- Weight loss. Once other health issues are eliminated, weight loss while training hard is a clear sign of inadequate energy intake (Manore, 2015). If an athlete wants to lose body fat and weight, this process should be planned at a time when exercise energy demands are lower and there is more time to focus on energy intake and food selection (Manore, 2013). Typically, it is not recommended that athletes diet for weight loss during periods of high-level training or during the competitive season. Finally, any focus on weight loss should emphasize the preservation of lean tissue while maximizing fat loss. Thus, diet composition during this time is as important as total energy intake. Adequate protein must be consumed to assure lean tissue is preserved (Longland et al., 2016; Mettler et al., 2010).
- Poor growth. For young athletes, if growth is below the recom-mended levels, it may be due to inadequate energy to fuel both exercise and growth. Poor growth may be most evident in high energy demanding sports (e.g., endurance sports) or weight sen-sitive sports (e.g., gymnastics, diving or dance).
- Frequent injuries/illnesses. Repeated muscle or bone injuries that heal slowly may also be a sign of overtraining and under fueling. The Female Athlete Triad (Nattiv et al., 2007) established the link between low EA, menstrual dysfunction and bone health issues in women. Subsequent research has confirmed this association (Barrack et al., 2014; Gibbs et al., 2013). Frequent illnesses may also be a sign of a weakened immune system due to inadequate energy intake and the nutrients important for immune health.
- Fatigue/irritability. If the athlete is finding it difficult to concentrate during exercise, or is shaky or lightheaded while training, it may be due to inadequate energy intake. This can be especially true if an athlete has not eaten for 3-4 hours before a training session, or if they do a long, hard run before eating breakfast.
In addition to the above health signs and symptoms, poor energy intake or food choices can dramatically affect overall nutrient intakes and status.
POOR MACRONUTRIENT INTAKES
The primary reasons for poor macronutrient intake, especially carbo-hydrate and protein, are due to poor energy intakes and/or poor food selection. Poor energy intakes can be due to purposeful energy or food restrictions, illness or injury, loss of appetite due to exercise training practices (Howe et al., 2014, 2016), or specific dietary practices (e.g., vegan diet). Poor food selection can be due to avoidance of particular foods or food groups (e.g., no processed or cooked foods), limited food availability or the inability to buy adequate food due to low income.
It is well documented that carbohydrate is important for exercise performance and to replenish liver and muscle glycogen stores following exercise (Thomas et al., 2016). It is generally recommended that athletes training very hard consume between 6-12 g carbohydrate/kg body weight/d (Thomas et al., 2016). Depending on body size and energy needs of the female athlete, this level of carbohydrate intake can be difficult for some to consume, especially if unprocessed, low energy dense carbohydrates are being consumed (e.g., whole fruits and vegetables, whole wet grains) (Hand et al., 2016). Overall, these types of carbohydrates are nutrient dense and are recommended as part of a healthy diet, but they are also filling, due to their high volume and high fiber content, which increases a sense of fullness and reduces hunger (Rolls, 2009). The result is that individuals consuming a low energy dense diet may eat fewer calories. Research suggests that low energy dense diets may be a contributing factor in the low EA and menstrual dysfunction seen in some endurance female athletes (Hand et al., 2016; Reed et al., 2011).
The female athletes most likely to be at risk for low protein intakes are vegans, who eliminate all animal products from their diet, and/or those female athletes who are dieting for weight loss (Cialdella-Kam et al., 2016). Thus, the primary focus needs to be on getting adequate, high quality protein spread out across the day (Thomas et al., 2016; Tipton & Witard, 2007). Current recommendations are that weight stable athletes consume 1.2-2.0 g protein/kg body weight/d (Rodriguez et al., 2009; Thomas et al., 2016). In addition, there is evidence supporting the intake of meals or snacks containing carbohydrate and protein after exercise for the preservation of lean tissue and glycogen replacement (Burke et al., 2017; Cialdella-Kam & Manore, 2009). Unfortunately, the majority of research on protein requirements of active individuals has been done in men.
Although research focuses on the need for adequate energy, carbo-hydrate and protein intakes, it is important that adequate total fat and essential fatty acids (linoleic acid and α-linolenic acid (ALA)) also be consumed. In the past, many female athletes avoided dietary fat, especially if they were interested in weight loss or maintaining a low body weight (Beals & Manore, 1998; Kopp-Woodroffe et al., 1999). In addition, athletes with low EA have been reported to have fat intakes less than the Dietary Reference Intake (DRI) of 20-35% of energy intake (Cialdella-Kam et al., 2014; Thomas et al., 2016). Dietary fat intakes less than 15% of energy intake increases the probability that intakes of essential fatty acids will be low, especially ALA (Manore, 2002). Most individuals consume adequate amounts of linoleic acid due to high amounts of vegetable oils in the diet, but intakes of ALA can be low if intakes of dark leafy vegetables, flax seed/oils, walnuts and soy products are limited. In addition, the conversion of ALA to eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) is low. These long-chain fatty acids are typically high in marine food and are important for numerous biological functions (Calder et al., 2010). Thus, if athletes follow a vegan diet and eliminate all marine and fish products from their diet, the intakes of EPA and DHA may be low. Emerging research has linked the importance of these two fatty acids for the attenuation of inflammation (Cialdella-Kam & Manore, 2017) and to brain health (Jackson et al., 2016), especially in sports or activities at high risk for concussion and brain injury (Bistrian et al., 2011).
POOR MICRONUTRIENT INTAKES AND STATUS
The micronutrient intakes of active women can be low if energy intake is restricted, food groups are eliminated, a special diet is followed (e.g., vegan, vegetarian or fad diet), the athlete has an eating disorder, or there are health issues that alter nutrient absorption (Cialdella-Kam et al., 2016; Manore, 2002, 2015). Female athletes are especially at risk for anemia due to low intakes of heme iron found in meat, increased iron losses in blood and urine, and iron sequestered due to inflammation. These factors can reduce the iron availability for red cell production. Other key blood nutrients that may be low in the diet of the female athlete are zinc, vitamin B-12 and folate. Meat, fish and poultry are high in heme iron, zinc and B-12, and contain a “meat factor” that helps the absorption of non-heme iron found in plant foods. Folate is high in whole grains, legumes, dark greens, fortified cereals and enriched breads. Diets high in processed foods may be low in iron, zinc, magnesium and B-vitamins (especially folate, B-6, riboflavin and thiamin). Athletes that eliminate dairy foods from the diet may have low intakes of calcium and vitamin D, since dairy is a source of these nutrients. Finally, athletes that exercise indoors will reduce production of vitamin D derived from sun exposure. Thus, it is important to assess the diet for appropriate blood (zinc, iron, B-12 and folate), energy (B-vitamins), and bone related nutrient intake (Cialdella-Kam et al., 2014, 2016; Woolf et al., 2013). Assessment of micronutrient status will involve examining food intakes, dietary patterns, access to food and clinical measures of blood and urine nutrient assessment markers where appropriate. If micronutrient status is low, health and performance will be compromised.
For the female athletes, micronutrients are most likely to be low if energy is low, food groups are eliminated, or highly processed foods make up the majority of the diet. The key micronutrients to monitor are the B-vitamins, vitamin D and selected minerals (zinc, iron, calcium, magne-sium). Conversely, active women with adequate energy intakes or those who use fortified/enriched foods or supplements appear to have good status (Woolf et al., 2017).
SUMMARY
A number of energy and nutrition issues may occur in the female athlete. However, if athletes are aware that they exist and know how to monitor their health, these issues can be addressed and corrected. Discussing their diet and nutrition issues with a qualified sports dietitian can help female athletes prevent nutrition problems before they arise.
REFERENCES
Arends, J.C., M.Y. Cheung, M.T. Barrack, and A. Nattiv (2012). Restoration of menses with nonpharmacologic therapy in college athletes with menstrual disturbances: a 5-year retrospective study. Int. J. Sport Nutr. Exerc. Metab. 22: 98-108.
Barrack, M.T., J.C. Gibbs, M.J. De Souza, N.I. Williams, J.F. Nichols, M.J. Rauh, and A. Nattiv (2014). Higher incidence of bone stress injuries with increasing female athlete triad-related risk factors: a prospective multisite study of exercising girls and women. Am. J. Sports Med, 42: 949-958.
Beals, K.A., and M.M. Manore (1998). Nutritional status of female athletes with subclinical eating disorders. J. Am. Diet. Assoc. 98: 419-425.
Beals, K.A., and M.M. Manore (2002). Disorders of the female athlete triad among collegiate athletes. Int. J. Sport Nutr. Exerc. Metab. 12: 281-293.
Bistrian, B.R., W. Askew, J.W. Erdman Jr., and M.P. Oria (2011). Nutrition and traumatic brain injury: a perspective from the Institute of Medicine report. J. Parenter. Enteral Nutr. 35: 556-559.
Bratland-Sanda, S., and J. Sundgot-Borgen (2013). Eating disorders in athletes: overview of prevalence, risk factors and recommendations for prevention and treatment. Eur. J. Sport Sci. 13: 499-508.
Burke, L.M., M.L. Ross, L.A. Garvican-Lewis, M. Welvaert, I.A.Heikura, S.G. Forbes, J.G. Mirtschin, L.E. Cato, N. Strobel, A.P. Sharma, and J.A. Hawley (2017). Low carbohydrate, high fat diet impairs exercise economy and negates the performance benefit from intensified training in elite race walkers. J. Physiol. 595: 2785-2807.
Calder, P.C., A.D. Dangour, C. Diekman, A. Eilander, B. Koletzko, G.W. Meijer, D. Mozaffarian, H. Niinikoski, S.J. Osendarp, P. Pietinen, J. Schuit and R. Uauy (2010). Essential fats for future health. Eur. J. Clin. Nutr. 64: S1-S13.
Cialdella-Kam, L., and M.M. Manore (2009). Macronutrient needs of active individuals: An update. Nutr. Today 44: 104-111.
Cialdella-Kam, L., and M.M. Manore (2017). Diet and exercise approaches for reversal of exercise-associated menstrual dysfunction. In: H.C. Lukaski (Ed.), Body Composition. Health and Performance in Exercise and Sport. Boca Raton, FL: CRC Press, pp. 357-374.
Cialdella-Kam, L., C.P. Guebels, G.F. Maddalozzo, and M.M. Manore (2014). Dietary intervention restored menses in female athletes with exercise-associated menstrual dysfunction with limited impact on bone and muscle health. Nutrients 6: 3018-3039.
Cialdella-Kam, L., D. Kulpins, and M.M. Manore (2016). Vegetarian, gluten-free, and energy restricted diets in female athletes. Sports 4: 50.
Gibbs, J.C., N.I. Williams, and M.J. De Souza (2013). Prevalence of individual and combined components of the female athlete triad. Med. Sci. Sports Exerc. 45: 985-996.
Gilliat-Wimberly, M., M.M. Manore, K. Woolf, P.D. Swan, and S.S. Carroll (2001). Effects of habitual physical activity on the resting metabolic rates and body compositions of women aged 35 to 50 years. J. Am. Diet. Assoc. 101: 1181-1188.
Guebels C.P., L.C. Kam, G.F. Maddalozzo, and M.M. Manore (2014). Active women before/after an intervention designed to restore menstrual function: resting metabolic rate and comparison of four methods to quantify energy expenditure and energy availability. Int. J. Sport Nutr. Exerc. Metab. 24: 37-46.
Hand, T.M., S. Howe, L. Cialdella-Kam, C.P. Hoffman, and M. Manore (2016). A pilot study: Dietary energy density is similar between active women with and without exercise-associated menstrual dysfunction. Nutrients 8: 230.
Hill, R., and P. Davies (2001). The validity of self-reported energy intake as determined using the doubly labelled water technique. Br. J. Nutr. 85: 415-430.
Hill, R.J., and P.S. Davies (2002). Energy intake and energy expenditure in elite lightweight female rowers. Med. Sci. Sports Exerc. 34: 1823-1829.
Howe, S.M., T.M. Hand, and M.M. Manore (2014). Exercise-trained men and women: role of exercise and diet on appetite and energy intake. Nutrients 6: 4935-4960.
Howe, S.M., T.M. Hand, T.M., D.E. Larson-Meyer, K.J. Austin, B.M. Alexander, and M.M. Manore (2016). No effect of exercise intensity on appetite in highly-trained endurance women. Nutrients 8: 223.
Jackson, P.A., V. Pialoux, D. Corbett, I. Drogos, K.I. Erickson, G.A. Eskes, and M.J. Poulin (2016). Promoting brain health through exercise and diet in older adults: a physiological perspective. J. Physiol. 594: 4485-4498.
Kopp-Woodroffe, S.A., M.M. Manore, C.A. Dueck, J.S. Skinner, and K.S. Matt (1999). Energy and nutrient status of amenorrheic athletes participating in a diet and exercise training intervention program. Int. J. Sport Nutr. 9: 70-88.
Longland, T.M., S.Y. Oikawa, C.J. Mitchell, M.C. Devries, and S.M. Phillips (2016). Higher compared with lower dietary protein during an energy deficit combined with intense exercise promotes greater lean mass gain and fat mass loss: a randomized trial. Am. J. Clin. Nutr. 103: 738-746.
Manore, M.M. (2002). Dietary recommendations and athletic menstrual dysfunction. Sports Med, 32: 887-901.
Manore, M.M. (2013). Weight management in the performance athlete. Nestlé Nutr. Inst. Workshop Series, 75: 123-133.
Manore, M.M. (2015). Weight management for athletes and active individuals: A brief review. Sports Med. 45: 83-92.
Manore, M.M., L.C. Kam, and A.B. Loucks (2007). The female athlete triad: Components, nutrition issues, and health consequences. J. Sports Sci. 25: 61-71.
Martin, M.K., D.T. Martin, G.R. Collier, and L.M. Burke (2002). Voluntary food intake by elite female cyclists during training and racing: influence of daily energy expenditure and body composition. Int. J. Sport Nutr. Exerc. Metab. 12: 249-267.
Melin, A., A.B. Tornberg, S. Skouby, S.S. Møller, J. Sundgot-Borgen, J. Faber, J.J. Sidelmann, M. Aziz, and A. Sjödin (2015). Energy availability and the female athlete triad in elite endurance athletes. Scand. J. Med. Sci. Sports 25: 610-22.
Mettler, S., N. Mitchell, and K.D. Tipton (2010). Increased protein intake reduces lean body mass loss during weight loss in athletes. Med. Sci. Sports Exerc. 42: 326-337.
Mountjoy, M., J. Sundgot-Borgen, L. Burke, S. Carter, N. Constantini, C. Lebrun, N. Meyer, R. Sherman, K. Steffen, R. Budgett and A. Ljungqvist (2014). The IOC consensus statement: Beyond the Female Athlete Triad-Relative Energy Deficiency in Sport (RED-S). Br. J. Sports Med. 48: 491-497.
Mountjoy, M., J. Sundgot-Borgen, L. Burke, S. Carter, N. Constantini, C. Lebrun, N. Meyer, R. Sherman, K. Steffen, R. Budgett and A. Ljungqvist and K. Ackerman (2015). Relative Energy Deficiency in Sport (RED-S) Clinical Assessment Tool (CAT). Br. J. Sports Med. 49: 421-423.
Nattiv, A., A. Loucks, M. Manore, C. Sanborn, J. Sundgot-Borgen, and M. Warren (2007). American College of Sports Medicine position stand: The female athlete triad. Med. Sci. Sports Exer. 39: 1867-1882.
Reed, J., J. Bowell, B. Hill, B. Williams, M. De Souza, and N. Williams (2011). Exercising women with menstrual disturbances consume low energy dense foods and beverages. Appl. Physiol. Nutr. Metab. 36: 382-394.
Rodriguez, N.R., N.M. DiMarco, and S. Langley (2009). Position of the American Dietetic Association, Dietitians of Canada, and the American College of Sports Medicine: Nutrition and athletic performance. J. Amer. Diet. Assoc. 109: 509-527.
Rolls, B.J. (2009). The relationship between dietary energy density and energy intake. Physiol. Behav. 97: 609-615.
Schulz, L., S. Alger, I. Harper, J. Wilmore, and E. Ravussin (1992). Energy expenditure of elite female runners measured by respiratory chamber and doubly labeled water. J. Appl. Physiol. 72: 23- 28.
Sjodin, A.M., A.B. Andersson, J.M. Hogberg, and K.R. Westerterp (1994). Energy balance in cross-country skiers: a study using doubly labeled water. Med. Sci. Sports Exerc. 26: 720-724.
Sundgot-Borgen, J., and I. Garthe (2011). Elite athletes in aesthetic and Olympic weight-class sports and the challenge of body weight and body compositions. J. Sports Sci. 29: S101-S114.
Sundgot-Borgen, J., N.L. Meyer, T.G. Lohman, T.R. Ackland, R.J. Maughan, A.D. Stewart, and W. Müller (2013). How to minimise the health risks to athletes who compete in weight-sensitive sports review and position statement on behalf of the Ad Hoc Research Working Group on Body Composition, Health and Performance, under the auspices of the IOC Medical Commission. Br. J. Sports Med. 47: 1012-1022.
Thomas, D.T., K.A. Erdman, and L.M. Burke (2016). Position of the Academy of Nutrition and Dietetics, Dietitians of Canada, and the American College of Sports Medicine: Nutrition and athletic performance. J. Acad. Nutr. Dietet. 116: 501-528.
Tipton, K.D., and O.C. Witard (2007). Protein requirements and recommendations for athletes: relevance of ivory tower arguments for practical recommendations. Clin. Sports Med. 26: 17-36.
Woolf, K., N.L. Hahn, M.M. Christensen, A. Carlson-Phillips, and C.M. Hansen (2017). Nutrition assessment of B-vitamins in highly active and sedentary women. Nutrients 9: 329.
Woolf, K., D.L. LoBuono, and M.M. Manore (2013). B Vitamins and the Female Athlete. In: Nutrition and the Female Athlete: From Research to Practice, 2nd Ed. 2013, pp 139-182. CRC Press, Boca Raton, FL..