Key Points
- Impaired Sweating: Athletes with spinal cord injuries (SCI) may have impaired sweating below the level of injury, limiting effective heat dissipation.
- Altered Blood Flow: Paralysis can lead to blood pooling in the lower limbs, affecting circulation and cooling.
- Wheelchair Use: Prolonged sitting in a wheelchair can reduce air circulation around the body, raising core temperature (Tcore).
- Hydration Challenges: Hydration management is complicated in SCI because of altered fluid distribution and retention. Athletes often have reduced thirst and thermal sensation responses, making hydration status harder to monitor.
- Medication Effects: Medication use in athletes with SCI may further influence hydration status, complicating fluid balance.
- Cooling Techniques: Combining hydration with cooling strategies (e.g., wearing cooling vests, applying hand cooling or ingesting ice slurries) will help regulate body temperature. Furthermore, combining portable fans with water sprays helps to simulate sweating and enhances evaporative cooling, compensating for athletes with SCI impaired ability to sweat and regulate body temperature.
Introduction
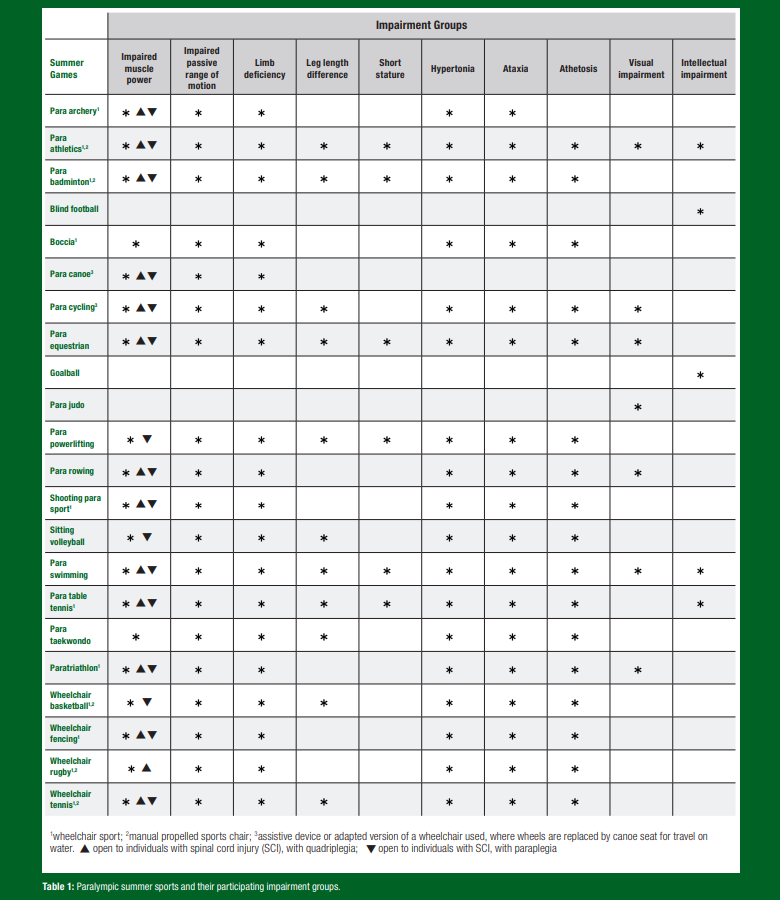
The Summer Paralympic Games has experienced remarkable growth, evolving into one of the largest multisport events globally, with 162 participating countries at the Paralympic Games in Tokyo (International Paralympic Committee, 2021). This expansion has led to an increased professionalism of both athletes and support staff (Paulson & Goosey-Tolfrey, 2017). As a result of this growth and the inclusion of a wider array of impairments across 22 summer sports (Table 1), there has become a greater emphasis on preparing the athletes for the challenging environments, particularly those related to heat (Alkemade et al., 2022). This need has become especially pressing given the recent games in Rio (2016), Tokyo (2020) and Paris (2024), where temperatures have exceeded 30 ℃ (Alkemade et al., 2022; Griggs et al., 2019; Mougin et al., 2024). The knowledge gleaned from the Olympic athlete is not directly transferable to the Paralympic athlete due to the unique physiological and thermoregulatory consequences of an athlete’s impairment (Paulson & Goosey-Tolfrey, 2017). For example, athletes with spinal cord injuries (SCI) have reached core temperatures (Tcore) exceeding > 39.5 ℃ during wheelchair rugby (WCR) game play in thermo-neutral environments ranging 18.4-20.9 ℃ (Griggs et al., 2017b). Para-triathletes have experienced Tcore > 40 ℃ during competitions held in a hot environment (33 °C air temperature, 35-41% relative humidity, 25-27 °C water temperature) with Tcore differences depending on athletes' race category and wetsuit use (Stephenson et al., 2020).
It is beyond the scope of this article to discuss the potential thermoregulatory challenges faced by all ten impairment groups and 22 sports shown in Table 1. Rather, this Sports Science Exchange (SSE) article is designed to provide a narrative review highlighting the thermoregulatory challenges faced by wheelchair athletes with SCI. It will: (i) highlight and discuss the findings of the available scientific literature related to thermoregulatory challenges during wheelchair sports and, (ii) provide practical examples of how the scientific literature can be applied.
What is a Spinal Cord Injury
Spinal cord injuries are often caused by trauma or congenital disorders, leading to varying degrees of motor, sensory and autonomic function loss (Jacobs & Nash, 2004). The extent of these losses depends on the lesion level and completeness. Cervical SCI affects all four extremities, whilst lower-level injuries in the thoracic or lumbar regions impact the legs and trunk muscles. Complete injuries cause total loss of sensory and motor communication between the brain and the tissue innervated below the lesion level, while incomplete injuries result in more varied outcomes, with some retaining partial function (Kirshblum et al., 2019).
Lesion level and completeness also influence autonomic nervous system function, essential for understanding altered cardiovascular, respiratory and thermoregulatory responses to exercise (Krassioukov, 2009). For example, in SCI, impaired blood return to the heart due to a lack of sympathetic vasoconstriction and an inactive muscle pump leads to decreased stroke volume and cardiac output, which is not compensated by an increased heart rate (HR) (Hopman, 1994). This results in long-term cardiac output reductions, especially in quadriplegia (~30% lower than able-bodied individuals, with a maximal HR of 110-130 b·min-1 (Jacobs & Nash, 2004)).
At the muscular level, SCI impairs sustained muscular contractions due to a reduced neurological stimulus, leading to muscle atrophy, reduced cross-sectional area and loss of muscle fibres (Janssen & Hopman, 2005). Muscle fibre composition shifts towards fast glycolytic, type II fibres, which are highly fatigable and alter contraction speed (Gerrits et al., 1999). Consequently, individuals with greater muscular atrophy, especially in higher lesions, report lower maximal oxygen consumption (V̇O2max) though training status and body mass still play a role (Janssen & Hopman, 2005).
Individuals with SCI are at a greater risk of heat illness compared with able-bodied counterparts due to a reduced afferent input to and efferent control of the thermoregulatory system (Price, 2006). Neural damage reduces sweating capacity and vasomotor control below the lesion. The severity of impairment is proportional with lesion level and completeness; those with quadriplegia and complete injury have less sensate skin, lower afferent input and reduced efferent response compared to lower-level paraplegia, limiting their ability to thermoregulate (Price, 2006).
Finally, individuals with a SCI > Thoracic 6 (T6) lesion level are at risk of experiencing life threatening episodes of hypertension, known as autonomic dysreflexia (AD). This can be triggered by bowel and/or bladder distension, spasms, pressure sores and even something as seemingly trivial as a tight shoelace or sitting on a sharp object. Therefore, AD should be considered when addressing thermoregulatory concerns and the reader is guided to Gee et al. (2015) for more information.
WHEELCHAIR SPORTS
The wheelchair sports currently receiving the most attention in the scientific literature are the court sports (i.e., basketball (WCB), tennis (WCT) and rugby (WCR)) (Paulson & Goosey-Tolfrey, 2017), although earlier research primarily focused on the exercise physiology of wheelchair racing (Bhambhani, 2002). Wheelchair court sports are characterised by short bouts of high-intensity exercise, lasting ~1 hr for WCB and WCR, while WCT matches range 1-3 hrs (Williamson et al., 2024). Wheelchair races vary from 100 m to marathon distances, with world-record marathon times of 1:17:47 hrs (2021) and 1:34:16 hrs (2023) for males and females, respectively. Paratriathlon has also gained increased attention (Stephenson & Goosey-Tolfrey, 2020[AK1] ), particularly since its inclusion at the Paralympics Games in 2016, with times of 57:51 min and 1:06:25 hrs recorded at Tokyo 2020 for male and female wheelchair categories, respectively. Separate male and female categories exist in WCB, WCT, wheelchair racing and paratriathlon, whereas WCR is a mixed sport with male and female athletes on the same team. Unlike WCB and WCR, wheelchair racing, WCT and paratriathlon take place outdoors, where heat becomes a significant factor influencing performance (Griggs et al., 2019).
Thermoregulatory responses during competition
Indoor sports like WCR and WCB present unique thermoregulatory challenges for athletes, particularly those with high-level SCI. Studies have shown that WCR players can reach Tcore exceeding 39.5 °C during game play, even in cool temperature-controlled sports arenas (Griggs et al., 2017b; O’Brien et al., 2022a). In one study, players with SCI experienced greater thermoregulatory strain than those without SCI, despite covering ~17% less distance and pushing ~10% slower on average (Griggs et al., 2017b). Under similar environmental conditions on the same sized court, WCB players with paraplegia, who experience lower thermoregulatory impairment, also face challenges. In a study by Griggs et al., (2015), both WCR players with quadriplegia and WCB players with paraplegia completed the same intermittent sprint protocol to replicate game play. WCR players showed a greater increase in Tcore, which continued to rise during recovery periods, indicating an inability to dissipate heat produced effectively. This was further demonstrated in a recent field study showing a similar Tcore response in WCB players when playing in hot vs temperate conditions (Grossmann et al., 2022). Despite this, Tcore exceeding 39.3 ℃ have been reported in female WCB players when competing in ~22 ℃ and 55% relative humidity (Logan-Sprenger & McNaughton, 2020). Thermoregulatory responses related to sex differences in wheelchair sports remains underreported, highlighting the need for further investigation.
Outdoor Paralympic sports, like WCT, endurance wheelchair racing and paratriathlon, are considered “high risk” events for thermoregulatory strain due to hot, humid conditions and athletes’ thermoregulatory impairments (Griggs et al., 2019). Endurance events such as paratriathlon often require high relative intensities sustained for a large portion of the race, elevating the risk of athletes developing whole body temperature elevations and/or heat illness (Stephenson et al., 2020). Further, intricacies within paratriathlon have also been shown to increase the risk of heat stress including impairment category and wetsuit use. For example, in a cohort of 28 para-triathletes (including wheelchair athletes) competing in Italy, where environmental conditions soared to 33 ℃, 41% relative humidity and 27 ℃ water temperature, 57% of those wearing wetsuits showed higher Tcore while swimming (Stephenson et al., 2020). This research contributed to the International Triathlon Union’s (ITU) safety risk categories for mitigating heat stress using wet-bulb globe and water temperatures. Moreover, it led to the publication of ‘Beat the Heat’ which guides both Olympic and Paralympic athletes (International Triathlon Union, 2019).
These increases in thermal strain in para sports described above necessitates specific strategies to ensure safety and performance, including tailored cooling methods, hydration protocols and continuous monitoring of thermal and physiological state.
PREPARING FOR THERMOREGULATORY STRAIN IN PARA SPORT
There has been growing emphasis by Paralympic practitioners to adopt both acute and chronic heat alleviation strategies to mitigate the effects of thermoregulatory strain and/or challenging environmental conditions on health and performance (Griggs et al., 2019). This section will highlight some heat mitigation strategies that have been trialled and reported in the scientific literature to gain that competitive edge.
Cooling Methods and Application
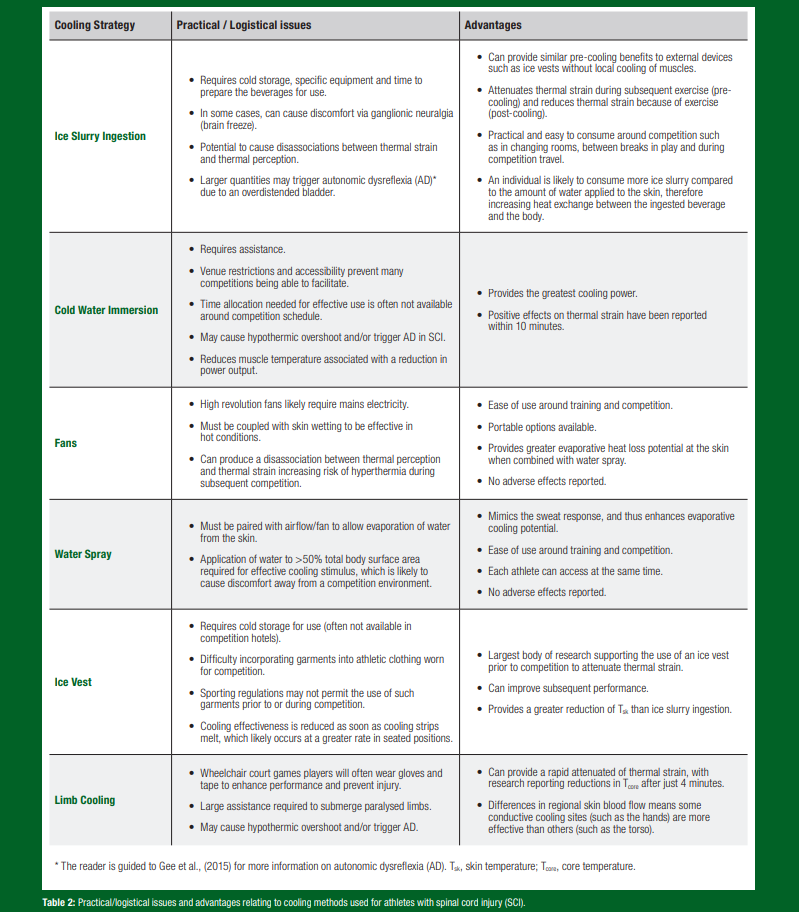
Common cooling methods used within able-bodied sporting events have also been explored within para-populations, with a focus on external cooling such as hand/foot cooling (Goosey-Tolfrey et al., 2008), ice vests (Webborn et al., 2010), and water sprays and fans (Griggs et al., 2017a). Hand cooling has been shown to reduce Tcore by ~0.5 ℃ compared to control and improved 3 km hand cycling performance, whilst ice vest application has shown mixed responses (Trbovich et al., 2014; Webborn et al., 2010). However, due to the practical and logistical issues and the lack of cooling power in some external cooling devices (Table 2), internal cooling has also gained traction using ice slurry ingestion in para-populations. For example, the use of ice slurry ingestion between sprint bouts (i.e., replicating the breaks in play in tennis), reduced Tcore by ~0.5 ℃ (Stephenson et al., 2022). Despite the potential for ice slurry ingestion to lower Tcore in para-populations, another study noted a delayed ice slurry induced reduction in Tcore from a hyperthermic state when evaporative and convective heat dissipation was limited (simulating SCI) (O’Brien et al., 2024). Therefore, ice slurry ingestion is likely best suited as a pre-cooling technique to offset the rise in Tcore rather than a rapid cooling method in response to hyperthermia or in response to an athlete with SCI overheating.
Timing and duration of cooling application are also important considerations to ensure maximum benefit without comprising athletes’ comfort or game routine. Increasing the athletes heat storage capacity and removal of heat before exercise (pre-cooling) and reducing the exercise induced rise in Tcore during an event (per-cooling) have both been studied in para-populations. Recent meta-analytical data provided evidence that pre-cooling methods have a greater capacity to influence thermoregulatory strain during subsequent events compared to applying per-cooling methods (O’Brien et al., 2022b). However, it should be noted that this could be due to the availability of more powerful cooling methods prior to competition compared to those available during competition. Therefore, a mixed method approach is likely best. This has been shown by Griggs et al. (2017a) who demonstrated pre-cooling using an ice vest and per-cooling using both water spray and fans provided a greater reduction in Tcore compared to no cooling or pre-cooling alone in SCI. Similarly, the use of both ice slurry ingestion and application of iced towels to the skin can reduce Tcore to a greater extent that ice slurry alone in WCB players with SCI at rest (Forsyth et al., 2016). Finally, consistent with thermoregulatory impairment, lesion level has been linked to cooling effectiveness, with greater benefits observed in individuals with quadriplegia (O’Brien et al., 2022b).
Heat Acclimation and Acclimatization
Performance decrements as a result of thermoregulatory stress can be ameliorated by use of heat acclimation or acclimatization described as the most important intervention one can adopt to offset the physiological strain of competing in the heat (Racinais et al., 2015). Heat acclimation refers to repeated exposures to artificial environments such as heat chambers whilst heat acclimatisation refers to exposure to natural environments such as warm weather training camps. Typical physiological benefits of heat adaptation include expansion of plasma volume, enhanced cardiovascular stability, improved sweat and skin blood flow response, improved fluid balance and improved thermal tolerance (Périard et al., 2015). As previously discussed, athletes with SCI often have reduced sweat and skin blood flow, making their ability to heat acclimate dependent on the level and completeness of their injury.
A typical protocol involves 7-14 days of repeated exposure to heat inducing an increase in Tcore, skin temperature and sweat response (if the athlete has a sweat response). A mixed active and passive heat acclimation protocol has been shown to be effective in para-triathletes (Stephenson et al., 2019). This study employed an 8-day protocol whereby for 5 days participants completed active heat acclimation sessions (45 min of exercise at 80% of max HR for two sessions and 90 min of exercise at 80% of max HR for 3 days), and 3 days with passive heat acclimation sessions (60 min rest following training) in a heat chamber set to 35 ℃ and 63% relative humidity. When completing a heat stress test following the heat acclimation protocol, para-triathletes experienced a 0.27 ℃ reduction in Tcore, with an ~13% increase in plasma volume compared to the pre-test, displaying evidence of partial heat acclimation (Stephenson et al., 2019). However, when selecting a protocol, it is important to consider the level of impairment. For example, the inability of athletes with SCI to sense heat through paralyzed limbs puts them at a greater risk of being unaware of their heat stress, and therefore careful monitoring is essential. Likewise, given the blunted HR response of a quadriplegic athlete with a complete lesion, a HR controlled protocol may be ineffective. Thus, taking a mixed method approach using both acute and chronic heat alleviation strategies will likely lead to the greatest reduction in thermoregulatory stress in para-athletes.
Hydration
Fluid intakes and sweat rates differ greatly during exercise dependent on lesion level and compared to other impairment types. For example, quadriplegic athletes consumed greater fluid volumes during exercise (60 min at 60% V̇O2max) in the heat (31 °C) than those with high and low-level paraplegia (764 ± 342, 472 ± 252 and 381 ± 251 mL, respectively) (Price & Campbell, 2003). Due to the increase in Tcore, an increased fluid consumption (especially cool/cold fluids) appears to help attenuate the thermal discomfort experienced during exercise (Stephenson et al., 2022). However, the combination of reduced sweating capacity and fluid loss and high fluid intakes in quadriplegic athletes (e.g., WCR players) can result in athletes gaining weight during exercise or more importantly experience episodes of hyponatremia. Additionally, medications commonly used by para-athletes (e.g., antispasmodics) may impair sweating and heat dissipation. Diuretics can disrupt fluid balance, increasing dehydration and/or electrolyte imbalance risks (Broad, 2019). Frequent, small sips are recommended to maintain hydration while avoiding excessive weight gain, preventing gastrointestinal discomfort and AD.
Practical Applications
- Education and Awareness: Educate athletes, coaches and support staff on impairment specific thermoregulatory responses whilst drawing attention to the signs and symptoms of heat illness, the importance of early intervention and effective heat mitigation strategies.
- Monitoring and Adjustments: Use wearable technology to continuously monitor Tcore, HR, and other physiological markers during training and competition. Adjust training intensity, duration and rest periods based on real-time data to prevent overheating and optimize performance.
- Adaptive Equipment: Utilize adaptive equipment designed to enhance heat dissipation and improve ventilation for wheelchair-bound athletes. Lightweight, breathable clothing and custom-designed wheelchairs with improved airflow can aid in thermoregulation.
- Hydration Protocols: Develop personalized hydration strategies based on individual sweat rates and environmental conditions. Encourage regular fluid intake before, during and after exercise to maintain hydration levels. Adaptive hydration tools, like long-straw bottles, are helpful for those with limited hand function or dexterity.
- Cooling Strategies: Implement pre-cooling techniques such as ice vests, ice slurries, cold-water immersion before exercise to offset the rise in core temperature. During training and competition, intermittent cooling breaks using fans, ice towels and/or misting sprays can help manage body temperature.
- Heat Acclimation: Para-athletes with SCI can benefit from heat acclimation protocols involving active and passive exposure to controlled heat environments. However, careful monitoring and a tailored approach are essential to ensure safety and effectiveness.
SUMMARY
Athletes with a SCI face heightened thermoregulatory challenges due to impaired sweating and vasomotor control, making them more susceptible to heat illness. The severity of these challenges is directly proportional to the injury’s level and completeness, with those having higher-level, complete injuries being most affected. Consequently, managing heat stress in SCI athletes is crucial for their safety and performance during sports. While hot and humid environments significantly increase risks, these challenges are also evident in indoor events, such as WCR, where despite competing in temperature-controlled sports halls, dangerous increases in Tcore have been reported due to the athletes’ impaired ability to dissipate heat.
The views expressed are those of the author and do not necessarily reflect the position or policy of PepsiCo, Inc.
References
Alkemade, P., H.A.M. Daanen, T.W.J. Janssen, E. Broad, V.L. Goosey-Tolfrey, T. Ibusuki, H. Kneepkens, J.D. Périard and T.M.H. Eijsvogels (2022). Heat preparedness and exertional heat illness in Paralympic athletes: A Tokyo 2020 survey. Temperature. 10:264–275.
Bhambhani, Y. (2002). Physiology of wheelchair racing in athletes with spinal cord injury. Sports Med. 32:23-51.
Broad, E. (ed.) (2019). Sports Nutrition for Paralympic Athletes, Second Edition (2nd ed.). CRC Press.
Forsyth, P., K. Pumpa, E. Knight, and J. Miller (2016). Physiological and perceptual effects of precooling in wheelchair basketball athletes. J. Spinal Cord Med. 39:671–678.
Gee, C.M., C.R. West, and A.V. Krassioukov (2015). Boosting in elite athletes with spinal cord injury: A critical review of physiology and testing procedures. Sports Med. 45:1133-42.
Gerrits, H.L., A. De Haan, M.T.E. Hopman, L.H.V. der Woude, D.A. Jones, and A.J. Sargeant (1999). Contractile properties of the quadriceps muscle in individuals with spinal cord injury. Muscle & Nerve. 22:1249–1256.
Goosey-Tolfrey, V., M. Swainson, C. Boyd, G. Atkinson, and K. Tolfrey (2008). The effectiveness of hand cooling at reducing exercise-induced hyperthermia and improving distance-race performance in wheelchair and able-bodied athletes. J. Appl. Physiol. 105:37–43.
Griggs, K.E., C.A. Leicht, M.J. Price, and V.L. Goosey-Tolfrey (2015). Thermoregulation during intermittent exercise in athletes with a spinal-cord injury. Int. J. Sports Physiol. Perform. 10:469–475.
Griggs, K.E., G. Havenith, T.A. Paulson, M.J. Price, and V.L. Goosey-Tolfrey (2017a). Effects of cooling before and during simulated match play on thermoregulatory responses of athletes with tetraplegia. J. Sci. Med. Sport. 20:819–824.
Griggs, K.E., G. Havenith, M.J. Price, B.S. Mason, and V.L. Goosey-Tolfrey (2017b). Thermoregulatory responses during competitive wheelchair rugby match play. Int. J. Sports Med. 38:177–183.
Griggs, K.E., B.T. Stephenson, M.J. Price, and V.L. Goosey-Tolfrey (2019). Heat-related issues and practical applications for Paralympic athletes at Tokyo 2020. Temperature 7:37–57.
Grossmann, F., C. Perret, B. Roelands, R. Meeusen, and J.L. Flueck (2022). Fluid balance and thermoregulatory responses during wheelchair basketball games in hot vs. temperate conditions. Nutrients. 14:2930.
Hopman, M.T.E. (1994). Circulatory responses during arm exercise in individuals with paraplegia. Int. J. Sports Med. 15:126–131.
International Paralympic Committee. (2021). Paralympic Games. https://www.paralympic.org/paralympic-games
International Triathlon Union, (2019). ‘Beat the heat’ accessible via https://www.triathlon.org/uploads/docs/HTB_v11.pdf
Jacobs, P.L., and M.S. Nash (2004). Exercise recommendations for individuals with spinal cord injury. Sport Med. 34:727–751.
Janssen, T.W.J., and M.T.E. Hopman (2005). Spinal cord injury. In J.S.Skinner (ed.) Exercise testing and exercise prescription for special cases: theoretical basis and clinical application. 3rd edition. Philadelphia: Lippincott Williams & Wilkins, pp 203–219.
Kirshblum, S.C., S.P. Burns, F. Biering-Sorensen, W. Donovan, D.E. Graves, A. Jha, M. Johansen, L. Jones, A. Krassioukov, M.J. Mulcahey, M. Schmidt-Read, and W. Waring (2011). International standards for neurological classification of spinal cord injury (revised 2019). J. Spinal Cord Med. 34:535–546.
Krassioukov, A. (2009). Autonomic function following cervical spinal cord injury. Respir. Physiol. & Neurobiol. 169:157–164.
Logan-Sprenger, H.M., and L.R. Mc Naughton (2020). Characterizing thermoregulatory demands of female wheelchair basketball players during competition. Res. in Sport Med. 28:256–267.
Mougin, L., V. Bougault, S. Racinais, M.L. Mountjoy, B. Stephenson, S. Carter, L.J. James, S.A. Mears, and L. Taylor (2024). Environmental challenges facing athletes, stakeholders and spectators at Paris 2024 Olympic and Paralympic Games: an evidence-based review of mitigation strategies and recommendations. Br. J. Sports Med. 58:870-881.
O’Brien, T.J., S.J. Briley, B.S. Mason, C.A. Leicht, and V.L. Goosey-Tolfrey (2022a). A high-intensity warm-up increases thermal strain but does not affect repeated sprint performance in athletes with a cervical spinal cord injury. Int. J. Sports Physiol. Perform. 17:440–449.
O’Brien, T.J., K.M. Lunt, B.T. Stephenson, and V.L. Goosey-Tolfrey (2022b). The effect of pre-cooling or per-cooling in athletes with a spinal cord injury: A systematic review and meta-analysis. J. Sci. Med. Sport. 25:606–614.
O’Brien, T.J., V.L. Goosey-Tolfrey, and C.A. Leicht (2024). Compromised heat loss leads to a delayed ice slurry induced reduction in heat storage. PLoS One. 19:e0305068.
Paulson, T., and V. Goosey-Tolfrey (2017). Current perspectives on profiling and enhancing wheelchair court sport performance. Int. J. Sports Physiol. Perform. 12:275–286.
Périard, J.D., S. Racinais, and M.N. Sawka (2015). Adaptations and mechanisms of human heat acclimation: Applications for competitive athletes and sports. Scand. J. Med. Sci. Sport. 25:20–38.
Price, M.J., and I.G. Campbell (2003). Effects of spinal cord lesion level upon thermoregulation during exercise in the heat. Med. Sci. Sports Exerc. 35:1100-1107.
Price, M.J. (2006). Thermoregulation during exercise in individuals with spinal cord injuries. Sport Med. 36:863–879.
Racinais, S., J.-M. Alonso, A.J. Coutts, A.D. Flouris, O. Girard, J. González-Alonso, C. Hausswirth, O. Jay, J.K.W. Lee, N. Mitchell, G.P. Nassis, L. Nybo, B.M. Pluim, B. Roelands, M.N. Sawka, J. Wingo, and J.D. Périard (2015). Consensus recommendations on training and competing in the heat. Br. J. Sports Med. 49:1164–1173.
Stephenson, B.T., and V.L. Goosey-Tolfrey (2020. Physiological considerations for paratriathlon training and competition. In: S. Migliorini (ed.) Triathlon Medicine. Berlin: Springer Nature.
Stephenson, B.T., K. Tolfrey, and V.L. Goosey-Tolfrey (2019). Mixed active and passive, heart rate-controlled heat acclimation is effective for paralympic and able-bodied triathletes. Front. Physiol. 10:1214.
Stephenson, B.T., S.P. Hoekstra, K. Tolfrey, and V.L. Goosey-Tolfrey (2020). High thermoregulatory strain during competitive paratriathlon racing in the heat. Int. J. Sports Physiol. Perform. 15:231–237.
Stephenson, B.T., T.J. O’Brien, M.J. Hutchinson, C. D'Angeli, A. Cockram, B.S. Mason, and V.L. Goosey-Tolfrey (2022). Ice slurry ingestion lowers thermoregulatory strain in wheelchair tennis players during repeated sprint intervals in the heat. Int. J. Sports Physiol. Perform. 17:1748–1755.
Trbovich, M., C. Ortega, J. Schroeder, and M. Fredrickson (2014). Effect of a cooling vest on core temperature in athletes with and without spinal cord injury. Spinal Cord Inj. Rehabil. 20:70–80.
Webborn, N., M.J. Price, P. Castle, and V.L. Goosey-Tolfrey (2010). Cooling strategies improve intermittent sprint performance in the heat of athletes with tetraplegia. Br. J. Sports Med. 44:455–460.
Williamson, S., C.L. Ardern, C. Berry, N. Heron, D.C. Janse van Rensburg, M.G.T. Jansen, S. McCormick, M. Reid, A. Sánchez-Pay, T. Saueressig, L.J. Schoonmade, R.B. Shaw, R.M.A. van der Slikke, N. Webborn, and B.M. Pluim (2024). The physical demands of wheelchair tennis match play: A systematic review with meta-analysis.
Sports Med. 54:1931–1953.